Citation
Barcala, X., Zaytouny, A., Rego-Lorca, D., Sanchez-Quiros, J., Sanchez-Jean, R., Martinez-de-la-Casa, J. M., Dorronsoro, C., & Marcos, S.; Visual simulations of presbyopic corrections through cataract opacification. Journal of Cataract & Refractive Surgery 2022, 10: 1097. For more information, click here.
Abstract
Patients can rank the perceived image quality through cataract up to high level of opacity and that the preoperative ranking of the corrections matches that performed postoperatively through transparent media.
Purpose
To study the viability of visual simulation of presbyopic correction in patients with cataract and the effect and impact of the cataract on the perceived visual quality of the different simulated presbyopic corrections preoperatively and postoperatively.
Setting
San Carlos Clinical Hospital, Madrid, Spain.
Design
Observational, noninterventional, pilot study, early feasibility of the device being studied.
Methods
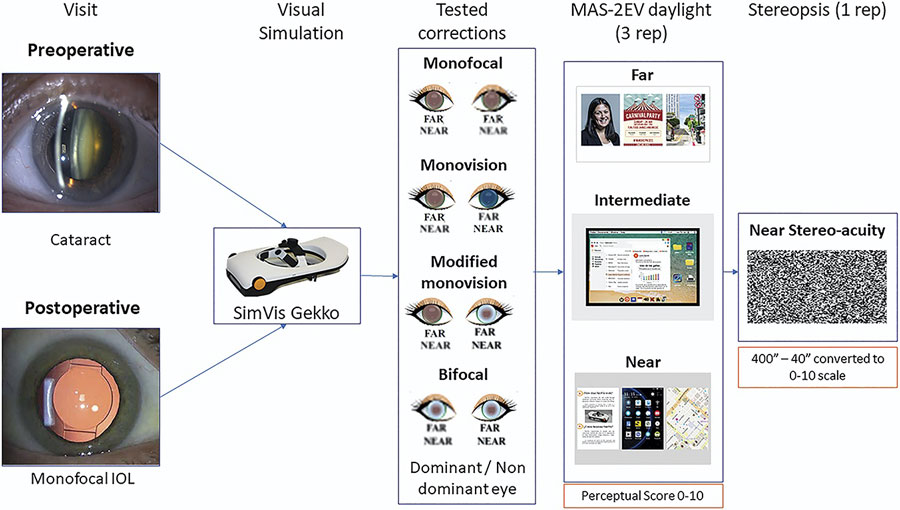
Cataract patients were tested preoperatively (n = 24) and postoperatively (n = 15) after bilateral implantation of monofocal intraocular lenses (IOLs). The degree of cataract was evaluated objectively with the objective scatter index (OSI). Visual acuity (VA) and perceived visual quality of natural scene images (Multifocal Acceptance Score) were measured before and after cataract surgery at far (4 m), intermediate (64 cm) and near distance (40 cm) with 4 binocular presbyopic corrections (single vision, bifocal, monovision and modified-monovision) simulated with a binocular Simultaneous Vision simulator based on temporal multiplexing.
Results
VA was significantly correlated with OSI (r = −0.71, P < .0005), although the visual degradation at far for each correction was constant and not correlated with OSI. The visual benefit at near distance provided by the presbyopic correction was noticeable (23.3% ± 27.6% across corrections) for OSI <5. The individual perceptual scores were highly correlated preoperatively vs postoperatively (r = 0.64, P < .0005) for all corrections and distances.